
Heart attack versus Cardiac arrest
Is there a difference between heart attack and cardiac arrest? People are frequently puzzled by these two terms because they are sometimes used interchangeably. A


Is there a difference between heart attack and cardiac arrest? People are frequently puzzled by these two terms because they are sometimes used interchangeably. A

Hormones are the chemical messengers in your body. Glands release hormones into your bloodstream, which work on various organs and tissues to control everything from

Serotonin can stave off depression and provide a feeling a euphoria When you’re happy and everything seems to be going well, you’re experiencing the impacts

Dopamine can provide an intense feeling of reward. Dopamine is most notably involved in helping us feel pleasure as part of the brain’s reward system.

Endorphins can also release stress and create a feeling of well-being. The body’s natural painkillers are endorphins. Endorphins are peptide hormones released by the hypothalamus

Oxytocin can help us bond with loved ones and can be released through touch, music and exercise. Oxytocin is a hormone that’s produced in the
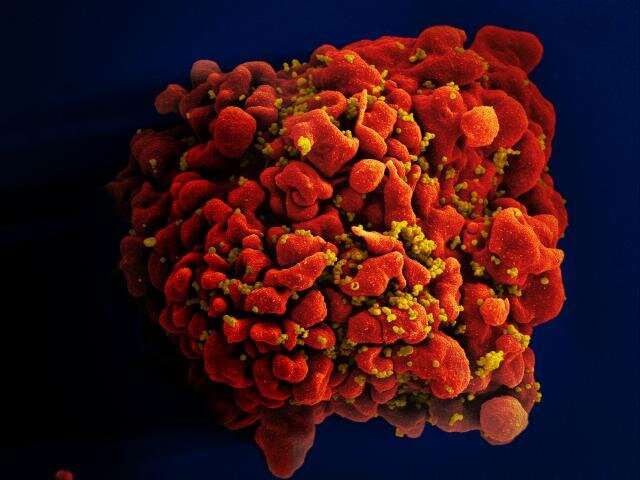
According to a presentation at the Conference on Retroviruses and Opportunistic Infections (CROI) on Tuesday 15th February, a woman with HIV who got a cord

Glaucoma is an eye illness that causes damage to the optic nerve, which can lead to visual loss that is permanent. It is one of

Bring 2021 Nobel Prizes into the classroom! From receptors for temperature and contact to organocatalysis. A compassionate voice of the consequences of colonialism to efforts
A girl who has lived 8 years of her life with a very uncommon genetic
Be the first to be notified by dropping your name and your active email address.